Depending on activity, location, and habitat, outdoor workers have the potential to encounter ticks and should take the appropriate precautions to prevent a bite and disease agents carried by infected ticks. According to the CDC, tick-borne disease cases more than doubled in the U.S. from 2004 to 2015, and since 2015, there have been approximately 50,000 cases reported each year. However, the number of cases is likely underreported, and the threat grows as the geographic ranges of ticks expands and new disease-causing pathogens are discovered.
Health Risks of Tick Bites
Tick-borne diseases can result in no symptoms, mild symptoms treatable at home, to severe infections requiring hospitalization. They can be extremely debilitating, life-threatening, and may result in long-term health problems or death. The diseases can be difficult to diagnose, so early recognition and treatment decrease the risk of serious complications. Clinical diagnosis is typically based on symptoms, physical examination, patient history (i.e., recent tick bite, exposure to areas where ticks are common, travel history), and tests. Test results may take several weeks, so providers may presumptively prescribe medications to treat the suspected illness. Risk factors include delayed treatment, age (being very young or old), a weakened immune system, and other serious health conditions.
Consult a physician if you experience any of the following symptoms suggestive of tickborne illness:
- Fever/chills: can experience a fever at varying degrees and times of onset.
- Nausea, vomiting, diarrhea, loss of appetite.
- Aches and pains: includes headache, fatigue, muscle aches, and joint pain. With Lyme disease, you may also experience joint swelling. The severity and time of onset can depend on the disease and the patient’s tolerance.
- Rash: Lyme disease, southern tick-associated rash illness (STARI), Rocky Mountain spotted fever (RMSF), Rickettsia parkeri rickettsiosis, ehrlichiosis, and tularemia can result in rashes with varying presentations.
- Necrotic lesions: an “inoculation eschar”, or scabbed region at the site of the tick bite.
- Tick paralysis (rare): thought to be caused by a toxin in tick saliva. Symptoms include impaired muscle control and paralysis starting in the feet and legs, moving upward. Symptoms typically develop after the tick has been attached for 3 to 7 days but subsides within 24 hours of removing the tick. Tick paralysis can become life-threatening if the tick is not removed and paralysis ascends to the torso.
Tick-borne diseases that may be transmitted from ticks in Illinois | Treatment |
Caused by bacteria: Anaplasmosis, Borrelia miyanmotoi disease (tick-borne relapsing fever), Ehrlichiosis, Lyme disease, Rickettsia parkeri rickettsiosis (a form of spotted fever), Rocky Mountain spotted fever (RMSF), Tularemia | Antibiotics. |
Caused by microscopic parasites: Babesiosis | Combination of antibiotics and anti-parasite medications. |
Caused by viruses: Bourbon virus disease, Heartland virus disease, Powassan virus disease | Supportive clinical management with medications used to treat symptoms and hospitalization required for severe disease. |
Cause unknown: Southern tick-associated rash illness (STARI) | Typically, antibiotics. |


Alpha-gal syndrome (AGS), also referred to as alpha-gal allergy, red meat allergy, or tick bite meat allergy, is a recently identified type of food allergy to red meat (beef, pork, lamb) and other products made from mammals (including some medications, cosmetics, vaccines, gelatin, and milk products). In the U.S., growing evidence suggests that AGS may be triggered by the bite of a lone star or blacklegged tick. In some people, this triggers an immune response that later produces mild to severe allergic reactions to red meat and other mammal products.Credt: CDC.
Identification
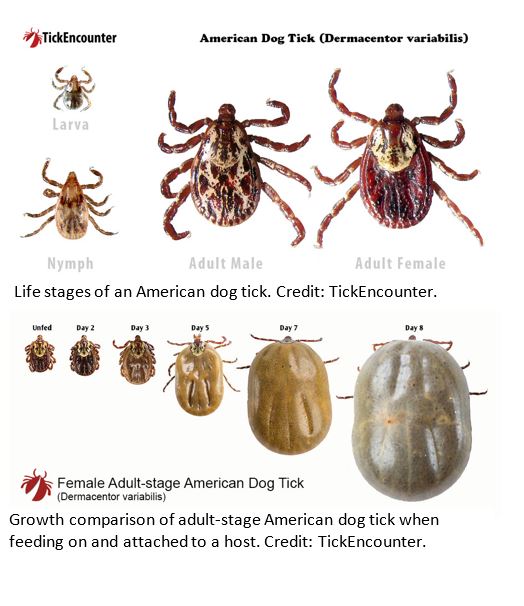
Ticks have four life stages: egg, larvae, nymph, and adult. Larvae, nymphs, and adult ticks may be encountered while working in the field; however, mainly nymphs and adults transmit disease agents. Ticks have flat, oval bodies, no wings, and tend to be reddish-brown or black, and sometimes have patterns. Larvae have six legs, while nymphs and adult ticks have eight legs. Ticks are very small and can be hard to spot. Depending on species, unfed adults range from ⅛- to ¼-inch (3-6 mm), engorged females are ½-inch or longer, and nymphs generally are 3∕64-inch (1 mm) long (size of a poppy seed). Larvae, nymphs, and adult females will increase size substantially and change color when feeding, becoming tan or gray-brown. In contrast, adult males feed very little, not growing in size, and attach primarily to animal hosts to find a female for mating.
At least 15 species of ticks occur in Illinois, but four that people are most likely to encounter:
- Blacklegged tick or ‘deer tick’ (Ixodes scapularis)
- Gulf coast tick (Amblyomma maculatum)
- Lone star tick (Amblyomma americanum)
Tick Identifications
Several apps and websites can provide free identifications based on up close and clear tick photos:
- For ticks encountered in Illinois, see the INHS Medical Entomology Lab website.
- For ticks encountered outside of Illinois, see the appendix.
Tick Bite Prevention
Before You Go Outdoors
- Ticks are most active spring through fall but can seek a blood meal year-round when the ground is dry, and the air temperature is above freezing.
- Ticks sit and wait in ankle- to chest-high grassy, brushy, woody vegetation by well-used paths.
Environment | Risk Level | Description |
Forested areas | High | Leaf litter and ground vegetation can harbor ticks. These habitats are home to many animals, which can maintain large tick populations. |
Agricultural lands | Moderate | Ticks can be found in edge habitats where crops and grasslands meet, often next to high-risk forested areas. |
Wetlands | Moderate | Ticks are not found directly in standing water; however, the vegetation surrounding the water can harbor ticks. |
Developed areas | Low | Well-maintained lawns seldom support large populations; however, ticks can survive in abandoned lots with tall grass and debris. |
Open water | Low | Vegetation surrounding water can harbor ticks and may be considered a moderate to high-risk habitat. |
- Ticks seek hosts by detecting breath (carbon dioxide) and body odors or sensing body heat, moisture, and vibrations.
- Ticks quest by holding onto the tips of leaves and grass and extending their first pair of legs in the air, waiting for a host to pass. When brushed by a moving animal or person, the tick will let go of the vegetation and climb onto the host. Ticks cannot fly or jump.
- Some ticks can also engage in pursuit and run across the ground if they detect a host.
- Walk in the center of trails and avoid brushing against or sitting in shrubby/grassy areas.
- While moving through grass, shrubs, or forest, perform a visual assessment every 10-20 meters (~20-40 steps at normal walking pace) by scanning your body from the chest down – front, back, and sides – then back up to your chest.
- Flick off loose ticks or capture them in a Ziploc bag or tape for disposal or ID.
- When leaving a field site, check your clothes and gear for ticks before getting in the vehicle, and remove as necessary.
Repellent Options and Application Guidance Document to learn about repellents and how to apply them. Always follow the directions on the label.
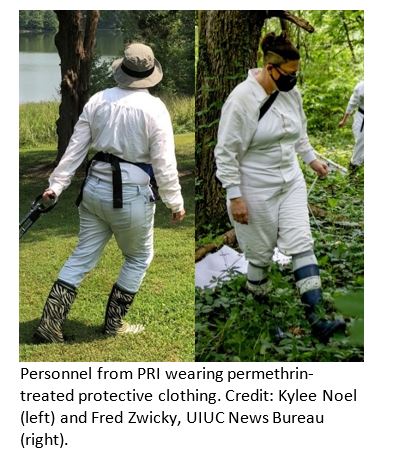
- Use pre-treated clothing or treat clothing and gear with products containing 0.5% permethrin.
- Wet permethrin is toxic to cats, fish, aquatic invertebrates, bees, and other beneficial insects. Take caution when applying it to clothing and gear.
- Use EPA registered insect repellents on skin.
- Wear light-colored clothing as it is easier to spot ticks.
- After grabbing onto a host, ticks tend to crawl upwards. Layer clothes from bottom to top, making an ascending barrier:
- Wear tall boots or hiking shoes.
- Tuck long pants into tight-weave socks.
- Wear a long-sleeved shirt tucked into pants.
- Pull hair up into a hat, or in braid or bun.
- Pro tip: Wrap double-sided tape around the top of boot.
- Ticks firmly attach to a host until removed or fully engorged with blood. Ticks become infected with bacteria, parasites, or viruses when feeding on infected hosts and can transmit these diseases through their saliva to future hosts during feeding.
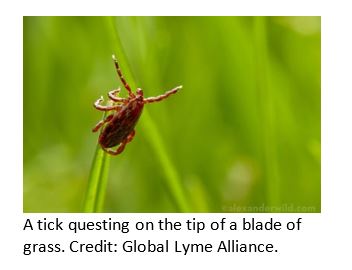
Questing Adult Tick. Credit: African Veterinary Information Portal.
After You Come Indoors
- If clothes require washing, use hot water, and then dry on high heat for at least 60 minutes. Otherwise, run dry or damp clothing in a dryer on high heat for 20 minutes.
- If laundry facilities are unavailable, shake your clothing far from where you will sleep, check it for ticks, and hang outside.
|
|
|
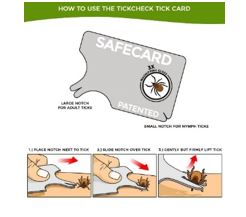
Tick Removal Methods
- Use clean fine-tipped tweezers or a commercial tick-removal device to grasp the tick around the mouthparts as close to the skin as possible.
- Pull upward with slow, steady, even pressure. Don’t squeeze, twist, or jerk the tick; this can cause the mouthparts to break off and remain in the skin. If this happens, remove the mouthparts with tweezers or leave it alone and let the skin heal.
- Never crush a tick with your fingers. Place the tick in a sealed bag or container and place it into a freezer to kill and preserve in case it is requested later by a medical or public health professional. Label the container with the name of the person the tick was attached to, date of removal, suspected location and date of exposure, and whether the person traveled outside their county of residence in past 10 days.
- Thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
How to remove a tick. Credit: NY State Dept. of Health.
Tick Removal Tools
These mechanical methods grasp the tick around its mouthparts rather than around the body and remove the tick using steadily increasing pressure. Note, they are applicable for removing nymphs and adults.
Ineffective Methods of Removal – “Debunked Myths”
- Application of chemicals (including gasoline, 70% isopropyl alcohol, fingernail polish, and petroleum jelly)
- Application of heat
- Injection or ingestion of medication (including antibiotics or local anesthetic)
Tick Testing
Although some commercial groups offer to test ticks for disease, in general, this is NOT recommended because:
- Labs that conduct tick testing are not required to have the high standards of quality control used by clinical diagnostic labs. Results of tick testing should not be used for treatment decisions.
- Positive results showing that the tick contains a disease-causing organism does not necessarily mean that you have been infected, and negative results can lead to false assurance as you may have been unknowingly bitten by another tick that was infected.
- If you have been infected, you will probably develop symptoms before the tick test results are available. If you do become ill, you should not wait for tick testing results before seeking treatment.
Instead, it is recommended that you keep any attached ticks preserved in case they are requested by a medical or public health professional later.
American Dog Tick or "wood tick" (Dermacentor variabilis)
Identification: Adults are reddish-brown, typically 3∕16-inch (5 mm) long, and have festoons. Females have a creamy-white scutum on their back and increase to ⅝-inch (15 mm) when engorged. Males have cream or gray-colored markings across their entire back and do not get much larger after feeding.

Behavior: Sit and wait predators that typically quest on ankle- to thigh-high vegetation. The highest risk of being bitten occurs during spring and summer. Research indicates they initiate questing behavior in high light intensity environments with low relative humidity.
Habitat: Wooded areas, forest/field edges, overgrown abandoned lots, fallow fields, roadsides, grassy edges of hiking trails, scrub along rivers/creeks.
Distribution: Considered well-distributed throughout Illinois. In the U.S., they are widely distributed east of the Rocky Mountains and occur in limited areas on the Pacific Coast.
Agents of Tularemia and Rocky Mountain spotted fever (RMSF).
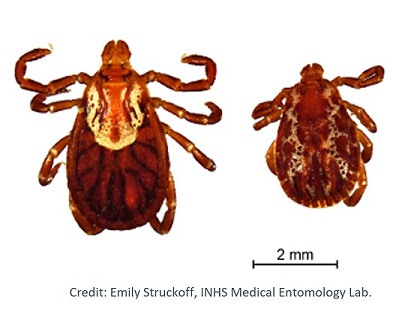
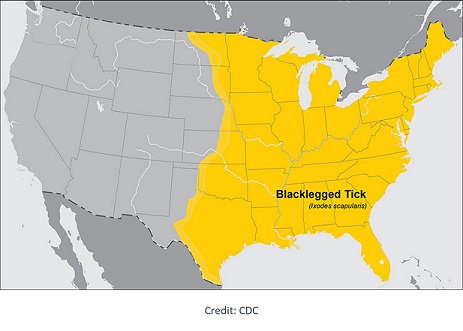
Blacklegged Tick or "deer tick" (lxodes scapularis)
Identification: Adults are reddish-brown to black, have dark legs, no festoons, and are typically less than ⅛-inch (3 mm) long unfed. Females have a dark brown or black scutum on their back and increase to ½-inch (13 mm) long when engorged. Nymphs are about the size of a poppy seed, 3∕64-inch (1 mm).


Behavior: They are generally sit and wait predators that typically quest on ankle- to thigh-high vegetation. Humans are most likely to be bitten spring through fall. However, adults may be active at temperatures above freezing, especially in sunny, warm microclimates.
Habitat: Need moisture and shade to survive. Strongly tied to humid microclimates and most often found in Illinois in mesic, upland, oak-hickory-dominated forests.
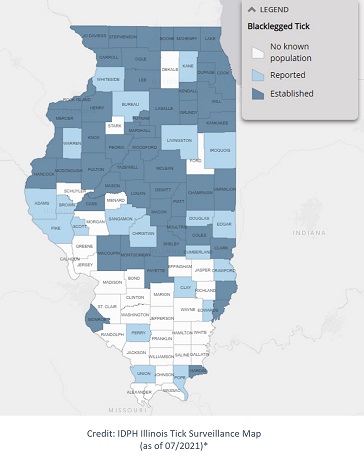
Distribution: Widely distributed across the eastern United States. Encountered throughout Illinois, but most prominent in the northern half of the state.
Agents of Anaplasmosis, Babesiosis, Borrelia miyamotoi disease (tick-borne relapsing fever), Ehrlichiosis, Lyme disease, and Powassan virus disease.
*CDC criteria for “established” ticks are at least six ticks or two life stages (larvae, nymph, adults) collected in a single year. Criteria for “reported” ticks are one to five ticks of the same life stage that have been identified.
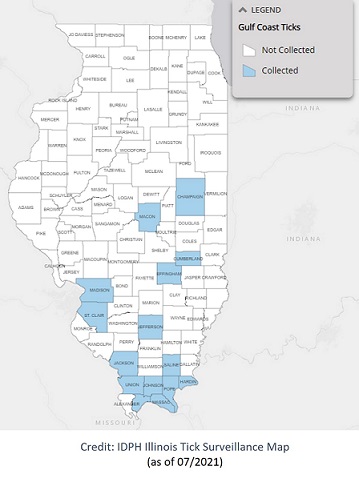
Gulf Coast Tick (Amblyomma maculatum)
Identification: They are distinguished by the very ornate markings on their reddish-brown bodies. Adults are typically ¼-inch (6 mm) long unfed and up to ½-inch (13 mm) or longer fully engorged. Adult males have clean, white lines in a web-like formation on the entire body and do not increase in size after feeding, and adult females have bright, white markings on the dorsal shield.
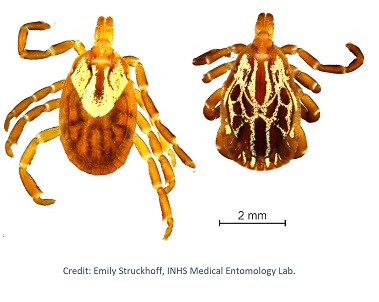
Behavior: Typically quest in ankle- to chest-high grass and vegetation to seek a passing host. Larvae and nymphs feed on birds and small rodents, while adult ticks feed on deer and other wildlife.
Habitat: Found in sunny environments with little to no canopy. Found in open habitats, including prairies, mowed and fallowed fields, roadsides, and near water sources.
Distribution: They can be found in coastal regions of the U.S. along the Atlantic coast and the Gulf of Mexico. Reports indicate very focal areas in central and southern Illinois and potentially moving northwards.

Agents of Rickettsia parkeri rickettsiosis, a form of spotted fever.
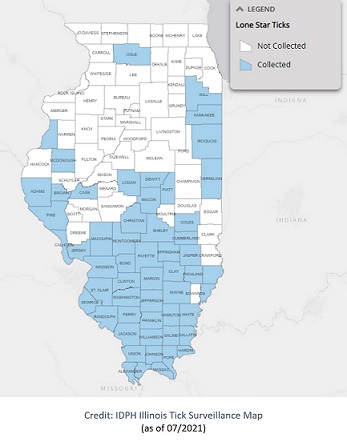
Lone Star Tick (Amblyomma americanum)
Identification: Adults are reddish-brown with prominent festoons. Adult females are distinguished by a white dot or “lone star” on their back and are typically ⅛-inch (3 mm) long unfed and ½-inch (13 mm) or longer and gray fully engorged. Adult males are slightly smaller than ⅛-inch (3 mm) and have light-colored patterns along the outer margins of the body.
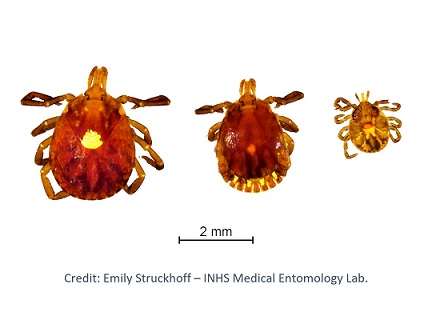
Behavior: Very aggressive sit and wait/ambush predators that bite humans. Their saliva can be irritating; redness and discomfort at a bite site do not necessarily indicate an infection. The nymph and adult females most frequently bite humans and transmit disease. The greatest risk of being bitten in early spring through late fall.
Habitat: Wooded areas, especially hardwood dominated – most common in secondary growth areas (e.g., forests with dense underbrush or in old field successional areas), especially along transitional zones such as vegetation or scrub along rivers/creeks near forest edge or between meadows and forest.
Distribution: Widely distributed across the Midwest, Southeast, and Eastern United States. Most dense in southern and central Illinois, but populations are increasing northwards; expected to be common throughout the state.
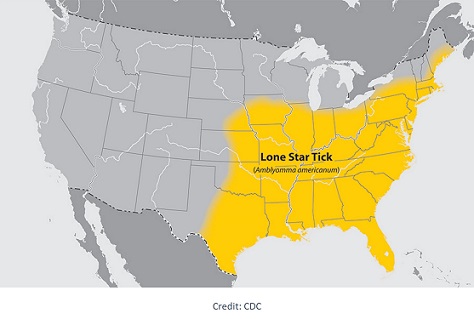
Agents of Alpha-gal syndrome (AGS, aka “red meat allergy”), Bourbon virus disease, Ehrlichiosis, Heartland virus disease, Southern tick-associated rash illness (STARI), and Tularemia.
Resources
- African Veterinary Information Portal – Questing tick video: https://www.youtube.com/watch?v=gGa6AkriVFw
- Alpha-gal Information: https://alphagalinformation.org/
- CDC – Ticks: https://www.cdc.gov/ticks/index.html
- CDC – Bourbon Virus Test: https://www.cdc.gov/amd/whats-new/bourbon-virus-test.html
- Columbia University Irving Medical Center – Tick Paralysis: https://www.columbia-lyme.org/tick-paralysis
- Cornell’s Insect Repellent Essentials: A Brief Guide: https://ecommons.cornell.edu/handle/1813/66722
- Dymond, N. and Swift, I. (2008) Permethrin toxicity in cats: A retrospective survey of 20 cases. Aust Vet J, 86: 219-23. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1751-0813.2008.00298.x
- Global Lyme Alliance – Questing Tick Photo: https://www.globallymealliance.org/blog/blood-water-infection-changes-tick-behavior
- IDPH – Common Ticks: https://www.dph.illinois.gov/topics-services/environmental-health-protection/structural-pest-control/common-ticks
- IDPH – Illinois Tick Surveillance Map: https://idph.maps.arcgis.com/apps/MapSeries/index.html?appid=976061db733441eb977ef5cf2facd5c4
- Illinois Lyme Association: https://www.illymeassociation.org/
- INHS Medical Entomology Program, Holly C. Tuten, PhD: https://medical-entomology.inhs.illinois.edu/bitemap/
- Mayo Clinic – Alpha-gal Syndrome: https://www.mayoclinic.org/diseases-conditions/alpha-gal-syndrome/symptoms-causes/syc-20428608
- Missouri Department of Conservation – Ticks: https://mdc.mo.gov/discover-nature/field-guide/ticks
- NPIC – Permethrin Technical Fact Sheet: http://npic.orst.edu/factsheets/archive/Permtech.html
- Pest World – Ticks of Illinois: https://www.pestworld.org/ticks-by-state/illinois/The University of Maine – Ticks of Maine: https://extension.umaine.edu/ticks/maine-ticks/
- Tick Removal Tools:
- ProTick Remedy: https://tickinfo.com/protickremedy
- TickEase: https://tickease.com/
- TickKeyTM: https://tickkey.com/
- TickCheck®:
- Tick Research Lab of Pennsylvania –
- Tick Identification Guide: https://www.ticklab.org/tick-identification
- The Tick Lifecycle: https://www.ticklab.org/blog/2020/12/01/the-tick-lifecycle/
Appendix
Free tick identification services by state:
- If you don’t see a resource listed, check with a county extension office or local or state health department.
- For identification of ticks from pictures, check out TickSpotters or TickCheck.
- Tick reporting “apps”: TickTracker, The Tick App, NCSU TickID, TAMU Tick App, eTICK (Canada), TickReport, Vermont Tick Tracker.
Alabama: The Great Alabama Tick Survey
Alaska: Alaska Submit-A-Tick program
Arizona: Arizona Extension handout on ticks; University of Arizona Insect Identification
Arkansas: The Arkansas Tickborne Disease Project
California: Labs offering tick IDs and/or testing
Colorado: Co. Dept Public Health tick information; Veterinarian submission of ticks to CDPHE
Connecticut: The Connecticut Agricultural Experiment Station Tick Submissions
Delaware: DNREC Tick Program
Florida: FL Health Dept. Tickborne Diseases page; UF Insect ID Lab
Georgia: Georgia DPH Tick ID
Hawaii: Agricultural Diagnostic Service Center
Idaho: Idaho Dept. HW tick information; UI Insect Identification Request
Illinois: The INHS Medical Entomology Lab Statewide Tick Surveillance Program
Indiana: Tick INsiders
Iowa: Iowa State University Medical Entomology Lab
Kansas: KSU Extension handout on ticks; Kansas State University Insect Diagnostics Program
Kentucky: KY CHFS page on ticks; University of Kentucky Insect Identification
Louisiana: LA Dept. Health page on ticks; Louisiana State University Insect Identification
Maine: Tick Testing for the People of Maine
Maryland: University of Maryland Tick Identifications
Massachusetts: Massachusetts Tick Identification and Testing Services
Michigan: Michigan Department of Health & Human Services Tick Identification
Minnesota: Minnesota Department of Health Tick Monitoring Program
Mississippi: Mississippi State Department of Health Vector Identification
Missouri: Missouri ticks and tick-borne pathogen surveillance
Montana: Montana DPHHS page on ticks
Nebraska: Tick-Tag-Go project
Nevada: Nevada DHHS Handout on Lyme; Nevada Department of Agriculture Entomology ID Services
New Hampshire: NH DHHS page on ticks; NH Dept. of Agriculture Tick ID form
New Jersey: NJ DH Vectorborne Diseases page; Monmouth Co. Tick Identifications
New Mexico: NM DOH page on ticks; Museum of Southwestern Biology Division of Arthropods
New York: New York Ticks Lab
North Carolina: NCDHHS Tick Identification Form
North Dakota: North Dakota Health Tick Surveillance
Ohio: Submit-A-Tick program
Oklahoma: OK DH tickborne disease page; Find local Extension office
Oregon: OHA Lyme page; Oregon Extension Tick ID services
Pennsylvania: Identify-My-Tick
Rhode Island: TickSpotters Program
South Carolina: No service – link to SCDHEC Diseases spread by ticks
South Dakota: No service – link to map of Ticks in South Dakota
Tennessee: TN DH tick-borne diseases page; UTN Insect ID service; TN Co. Extension Offices
Texas: DSHS Tick Submission and Testing
Utah: UT DH Lyme page; Utah Plant Pest Diagnostic Lab
Vermont: Passive Tick Surveillance Program
Virginia: Fairfax Co. Tick Identification; No statewide service – link to VA DH tick flyer
Washington: Washington State Dept. of Public Health Tick Identification
West Virginia: No service – link to WV DHHR tick information and identification service for veterinarians
Wisconsin: University of Wisconsin Tick Identification; University of Wisconsin Insect Diagnostic Lab
Wyoming: WY DH tick information; University of Wyoming Extension Arthropod Identification Service